Based on data from Singapore’s National Cancer Centre, prostate cancer is the most commonly diagnosed cancer among men in Singapore. The prevalence of prostate cancer is particularly significant among men over the age of 50 years, but younger individuals with certain risk factors are also at risk.
Despite the high prevalence, various treatment options to manage prostate cancer are available. Early detection of prostate cancer can also increase the possibility of full recovery. To be able to identify prostate cancer during its early stages, patients may choose to undergo prostate screening. Unfortunately, there are still misconceptions spreading around about prostate screening that make patients misunderstand its role and function.
This guide aims to provide a better understanding of prostate cancer screening. Patients should make informed decisions about managing their overall well-being.
Prostate cancer screening is the first line of defence against prostate cancer and usually consists of two particular methods of testing:
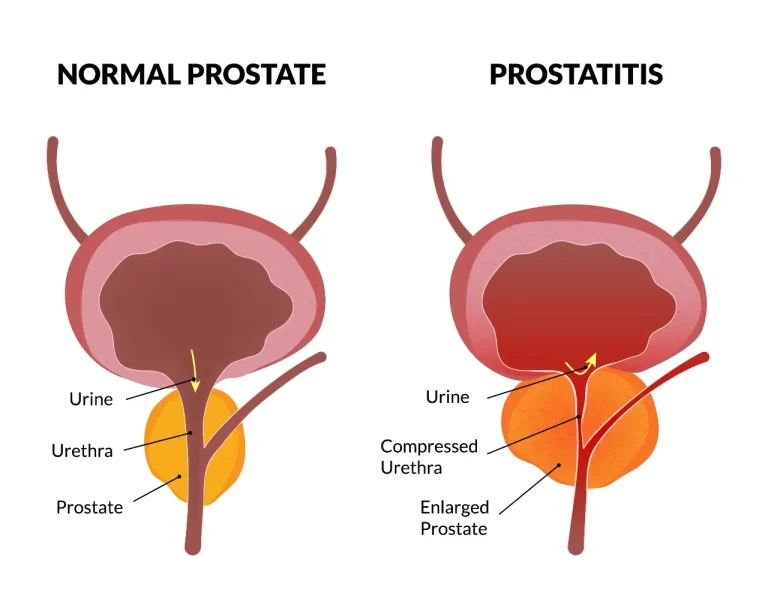
Prostate-Specific Antigen (PSA) Test: A blood test that measures the levels of PSA, a unique protein produced by the prostate gland. Elevated PSA levels may indicate the presence of prostate cancer or other prostate-related conditions.
Digital Rectal Examination (DRE): A physical examination done by a urologist where they check the prostate gland for lumps or abnormalities.
Both the PSA test and the DRE are quick and easy testing methods that can help assess your current prostate gland health and condition.
Early detection of prostate cancer can significantly improve treatment options and outcomes for patients. When the cancer has been successfully identified in its initial stages, the prostate cancer is often still localised to the prostate gland. Early detection of prostate cancer also allows patients to have more treatment options, such as surgery, radiation therapy, ablation therapy or active surveillance. When prostate cancer spreads to other parts of the body, it becomes more challenging to treat and can be detrimental to a patient’s health.
It is recommended that men aged 50 years and older should at least consider regular prostate screening after consultation with their doctors. However, men with higher risk factors of prostate cancer should also consider beginning screening earlier, typically around the age of 45. Click here to read more information about the risk factors of prostate cancer. If you’re not sure when to begin screening for prostate cancer, you can always schedule a consultation with a urology specialist at Assure Urology & Robotic Centre.
Common Misconceptions about Prostate Screening
Despite the clear benefits of prostate screening, there are still several misconceptions spread about the topic. Thus, men are discouraged from taking this crucial health check-up. Let’s debunk some of the most common myths surrounding the topic of prostate cancer screening:
Misconception 1: “Prostate cancer screening is unnecessary if I am well.”
One of the common misconceptions about prostate cancer screening is that it is only necessary to be taken by men who feel unwell or experience specific symptoms. However, early-stage prostate cancer is often asymptomatic, where it does not cause direct discomfort to the patient. By undergoing prostate cancer screening, patients might be able to identify prostate cancer before symptoms arise. Thus, prostate cancer screening enables patients to have the opportunity for timely intervention. It is also known that men diagnosed with early-stage prostate cancer have significantly higher survival rates than those diagnosed at more advanced stages.
Misconception 2: “PSA tests are always accurate.”
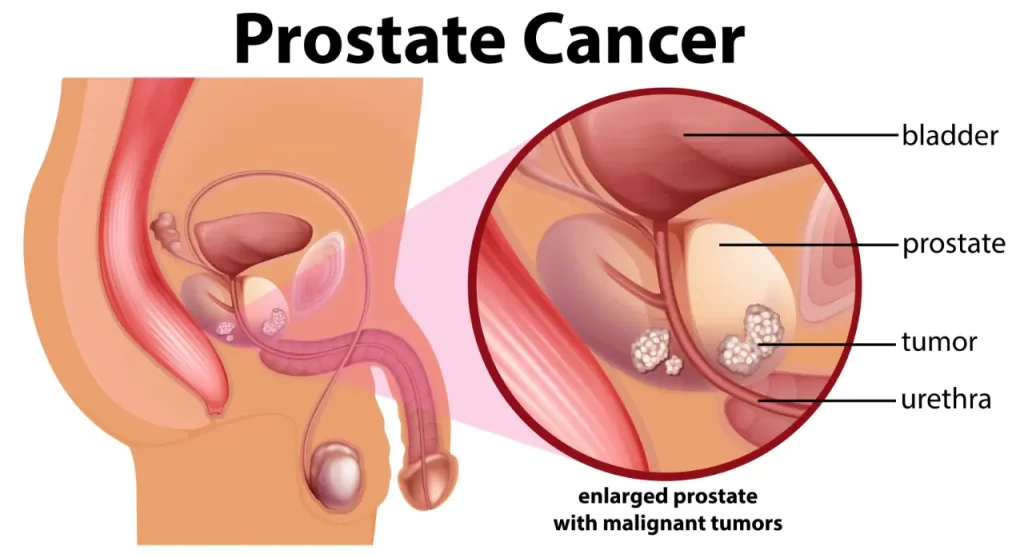
While the PSA test is a key component in prostate cancer screening, it can also give false results at times. False results like false positives and negatives can occur due to various factors. For instance, elevated PSA levels may result from prostatitis (inflammation of the prostate gland) or hiperplasia prostat jinak (BPH), which is an enlargement of the prostate gland. Similarly, some men with prostate cancer may show normal PSA levels. The limitations that come with the PSA test emphasise the importance of follow-up tests to confirm initial results. Imaging tests like MRI scans, or biopsies are often used to analyse PSA results further and ensure an accurate diagnosis. Consulting with a urologist is an essential step to understanding the implications of PSA test results and planning the next steps of treatments.
Misconception 3: “Screening leads to overdiagnosis and overtreatment.”
Some patients worry that prostate cancer screening might lead to receiving unnecessary treatments for slow-growing cancers that might not cause immediate problems for the patient. While this is a valid concern, urologists can address it through active surveillance. Instead of starting treatments to target the slow-growing cancers, patients are monitored through regular check-ups and tests. This approach allows timely intervention if the cancer progresses while avoiding potential side effects from unnecessary treatments. It is often better to know the presence of the cancer and choose the appropriate management option than not knowing it at all.
Misconception 4: “Only older men need to be screened.”
While prostate cancer is more common in men aged 50 and above, it is not exclusive to this age group. Men with higher risk factors can increase the likelihood of developing prostate cancer at a relatively younger age. Risk factors may include a family history of prostate cancer, genetic mutations (BRCA1 or BRCA2), lifestyle choices, smoking, diet, exposure to cadmium, and also Human Papillomavirus-16 (HPV-16). Men with these risk factors should consult a urologist to determine an appropriate screening schedule, regardless of age. Personalised screening plans ensure that those at higher risk can receive the care they need.
Misconception 5: “Prostate cancer is not a serious disease.”
It is essential to understand that not all prostate cancers progress slowly. Some types can be aggressive and may quickly spread to other body parts like the bones or lymph nodes. If patients continue to ignore the signs and symptoms of prostate cancer, their health and well-being might face severe consequences. Early detection through regular screenings offers the best chance of successful treatment and a higher quality of life. By staying informed about the potential risks and benefits of prostate cancer screening, patients can make informed decisions about their health and take proactive steps to protect themselves.
Schedule an Appointment with an Experienced Urologist in Singapore

Prostate cancer screening is a critical step in maintaining overall well-being. Debunking misconceptions about screening can help dispel fears and encourage men to be more aware of their health condition. If you or a loved one have questions about prostate health or are considering screening, schedule a consultation with our experienced team at Assure Urology and Robotics Centre led by Senior Consultant Urologist Dr Terence Lim. Take control of your health today because prevention and early actions are always better.


