Andrology refers to a branch of urology that has to do with disorders of the male reproductive system. Sexual health is important, so it is vital to get treated as early as possible if you feel like you may be experiencing andrological issues. Many of these conditions can be managed via conservative treatments or surgical intervention.
Read on to find out more about common andrology conditions.

Andropause (commonly termed ‘male menopause’) is a condition that involves a drop in testosterone levels in males and generally begins at the age of 40. This can cause a lowered sex drive, moodiness, and a variety of health issues, such as osteoporosis and metabolic syndrome.
Testosterone plays a huge role in male sexual and reproductive health, such as sperm production and sex drive. Testosterone levels are controlled closely via a feedback loop in the brain. When too much testosterone is produced, the brain sends signals to the pituitary gland, which, in turn, sends signals to the testes to reduce the production of testosterone.
Having too much or too little testosterone in one’s body can also result in health issues.
For example, having abnormally high levels of testosterone can result in low sperm counts, prostate enlargement, as well as mood swings. Having low levels of testosterone can result in low sex drive, small testicles, reduced sperm count or infertility.
Signs and symptoms of andropause include:
The doctor will take a blood sample to help determine the testosterone levels as well as other hormone levels. Next, your doctor will review your symptoms and your medical history. You can also expect a physical examination by your doctor.
Testosterone replacement therapy is often the treatment that your doctor may suggest, especially if there are certain conditions such as sexual dysfunction, type 2 diabetes or obesity (body-mass index higher than 30).
The benefits associated with testosterone replacement therapy include:
The risks associated with testosterone replacement therapy include:
Erectile dysfunction, also known as ED, is a condition whereby the man struggles to get or maintain an erection during sex. While it may be normal to experience problems with erections occasionally, ED occurs routinely during sexual intercourse.
ED can be caused by a number of factors, such as:
ED may arise from certain risk factors such as:
Your doctor will first review your medical history and do a physical examination. He or she may also order some blood tests. These blood tests may include a complete blood count, liver and kidney function tests, lipid profile, thyroid function tests and blood hormone levels.
Your doctor may also choose to conduct one or more of the following tests to help him or her with his or her diagnosis:
ED can be treated in 3 different ways, namely medication, shockwave therapy and surgery.
The most common medications used to help with ED are known as phosphodiesterase-5-inhibitors (PDE5I). Examples of PDE5I are sildenafil (Viagra), vardenafil (Levitra) and tadalafil (Cialis). They can help in treating ED by increasing the blood flow to the penis, allowing you to get an erection.
However, medications might not be recommended under the following circumstances:
Some side effects may include flushing, headaches and indigestion.
Shockwave therapy uses low-intensity and targeted sound waves to stimulate the growth of new blood vessels and improve the blood flow in the penis, which helps men to get an erection. This treatment is only suitable for vasculogenic ED.
A doctor will apply a set amount of shocks per minute for a fixed amount of time. Multiple sessions 2 to 3 weeks per week may be required. Generally, clinical improvements may take up to 3 months to be evident.
Side effects of shockwave therapy may include bruising of penile skin, blood in urine and painful erection.
A surgery can also be done to insert a penile implant. This is typically done when medications do not work.
A penile implant is an inflatable implant consisting of a reservoir, two cylinders and a pump that is being placed into the body. The two cylinders are placed in the penis and connected by tubing to the reservoir of fluid, which is implanted under the lower abdominal muscles. A pump is inserted under the loose skin of the scrotal sac between the testicles.
The man can inflate the prosthesis by pressing on the pump. To deflate the prosthesis, he can press the deflation valve at the base of the pump, which deflates the penis.
Premature ejaculation is defined as consistent ejaculation within 1 minute or less of vaginal penetration in at least 75%-100% of the times of sexual intercourse over a period of at least 6 months, resulting in clinically significant distress, sexual frustration, dissatisfaction, or tension between partners.
While premature ejaculation may occur from time to time, experiencing premature ejaculation consistently may indicate an underlying issue and can negatively affect sexual relationships between couples.
The exact cause of premature ejaculation is not known. However, some common causes of premature ejaculation may include:
Risk factors of premature ejaculation include:
Some treatments available to help with premature ejaculation are behavioural therapy and medications.
Behavioural therapy or psychotherapy can help men with premature ejaculation by emphasising control of ejaculation by learning new techniques, encouraging better communication as well as reducing anxiety and increasing confidence.
Therapy is best used in couples where premature ejaculation is caused by performance anxiety.
Some medications that can help with premature ejaculation include:
Infertility in men may occur due to a number of reasons, such as low sperm production, abnormalities in sperm functions, illnesses, injuries and even lifestyle changes. This results in lower chances of impregnating their female partners. In Singapore, 15% of Singaporean couples have difficulty getting pregnant, and 50% of these couples are due to male infertility.
Causes of male infertility include:
Some of the risk factors to take note of include:
A spermiogram involves the sampling of semen and sending it for analysis at the laboratory. This helps evaluate male fertility.
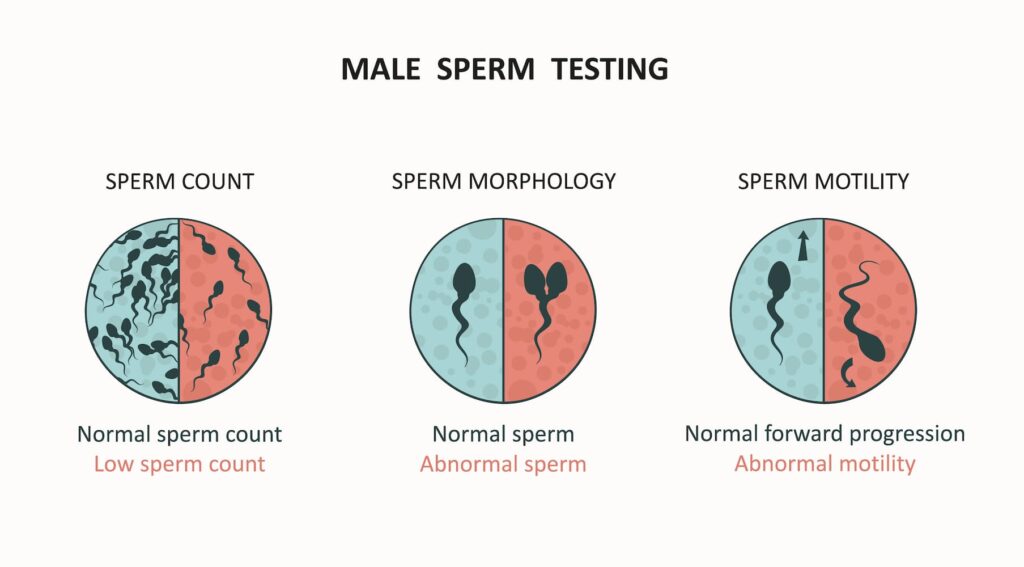
Things that the analysis will show include:
A hormone assay involves collecting a blood sample and sending it for analysis at the laboratory.
Hormones that are sampled include:
An ultrasound of the scrotum can be done. This allows the doctor to detect any problems, such as an unusual mass in the scrotum, damage to tissues or structures, as well as any abnormal swelling or inflammation of the testes.
A varicocele is an enlargement of the veins within the loose bag of skin covering the testicles. These can cause some discomfort or pain. A varicocele may also affect the development of the testicles and result in low sperm count or infertility. If left untreated, it may lead to 3 main problems:
A varicocele usually does not require treatment. However, for men who are experiencing infertility due to a varicocele, surgery may be recommended as part of the fertility plan.
A varicocelectomy involves the removal of varicoceles by cutting the veins and closing off the ends. This helps restore blood flow to the scrotum, which, in turn, increases sperm and testosterone production.
A semen analysis can be done post-surgery to discern whether fertility improves.
Penile curvature, also known as Peyronie’s disease, is a condition whereby scar tissues form under the skin of the penis. The scar tissues pull on the surrounding tissues and cause the penis to curve or bend. This can make erections painful, which can affect sexual intercourse.
Penile curvature can occur due to:
Penile curvature refers to the condition where the penis is curved during an erection. Penile curvature surgery helps to correct this curvature. However, it is usually only recommended for severe patients who do not respond to non-surgical treatments.
There are several techniques used in penile curvature surgery, namely:
A varicocelectomy involves the removal of varicoceles by cutting the veins and closing off the ends. This helps restore blood flow to the scrotum, which, in turn, increases sperm and testosterone production.
A semen analysis can be done post-surgery to discern whether fertility improves.
All in all, many andrological issues can be treated or managed. The most important thing is to seek professional help as soon as possible if you feel like you may be suffering from an andrological condition.

MBBS, MRCSed, MMED(Surgery)
Dr Terence Lim is a Senior Consultant Urologist with a subspecialty in Uro-Oncology. He is also the Medical Director at Assure Urology & Robotic Centre. His clinical interests include Uro-Oncology, Minimally-invasive Urological Surgery, Urinary Stone Disease, Endourology and Prostate Health.
Prior to his private practice, Dr Terence Lim spent almost two decades in public healthcare. He served as the Senior Consultant and Chief of the Department of Urology at Changi General Hospital (CGH). In addition, he is currently a Visiting Consultant at CGH. Dr Lim was also the director of CGH’s Advanced Surgical Centre, a committee dealing with complex surgeries, including robotic surgeries.
Your health is important to us and some conditions require immediate attention. For emergencies, please contact us at 9835 0668.

MBBS, MRCSed, MMED(Surgery)
Dr Terence Lim is a Senior Consultant Urologist with a subspecialty in Uro-Oncology. He is also the Medical Director at Assure Urology & Robotic Centre. His clinical interests include Uro-Oncology, Minimally-invasive Urological Surgery, Urinary Stone Disease, Endourology and Prostate Health.
Prior to his private practice, Dr Terence Lim spent almost two decades in public healthcare. He served as the Senior Consultant and Chief of the Department of Urology at Changi General Hospital (CGH). In addition, he is currently a Visiting Consultant at CGH. Dr Lim was also the director of CGH’s Advanced Surgical Centre, a committee dealing with complex surgeries, including robotic surgeries.
Your health is important to us and some conditions require immediate attention. For emergencies, please contact us at 9835 0668.
No issue is too small. Contact any of our friendly staff and we will get back to you as soon as possible.
Reach out to us for expert urological care.
For enquiries, leave a message and our friendly team will get in touch with you.
For urgent enquiries after office hours, call or WhatsApp us at (65) 9835 0668.
Monday – Friday: 9:00AM – 5:00PM
Saturday: 9:00AM – 12:30PM
Sunday & Public Holiday: CLOSED

© 2023 All Rights Reserved | Assure Urology & Robotic Centre | Terms & Conditions