The prostate gland is part of the male reproductive system, and its main job is to produce fluid in semen that provides nutrition for the sperm. The development of the prostate gland is controlled by testosterone, a male hormone.
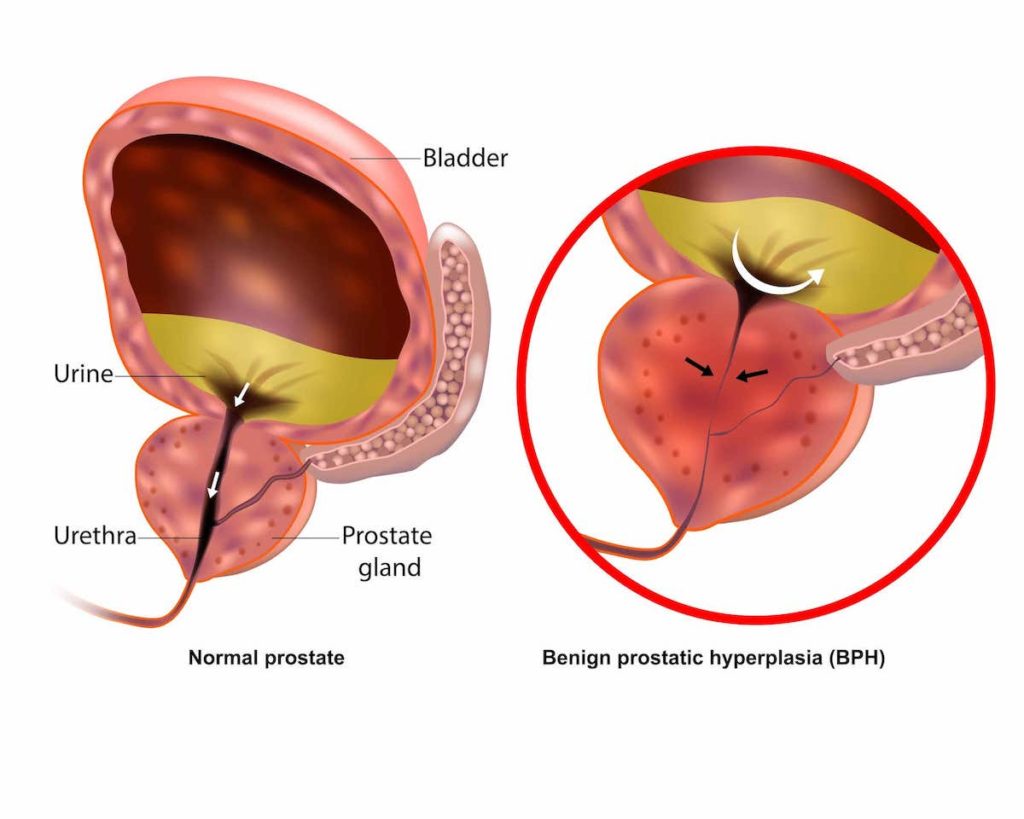
The prostate gland usually goes through 2 phases of growth during a man’s life — the first begins early on during puberty when the prostate gland doubles in size. The second phase starts around age 25 and continues as they age. The condition in which the prostate gland enlarges to more than 20-25 g is known as benign prostatic hyperplasia (BPH).
Benign prostatic hyperplasia is a very common condition affecting most males worldwide. Its prevalence increases after the age of 40 and reaches around 70-80% at the age of 90. Additionally, according to a study conducted on benign prostatic hyperplasia in Singapore, it was observed that with the population ageing, there is potential for the condition to become one of the most common urological conditions in the country.
BPH is a benign condition, which means it is not cancerous and will not increase the risk for prostate cancer. BPH itself may not need any treatment, but it can often cause several serious urinary symptoms that may warrant medical intervention when it affects your daily life.
BPH can lead to lower urinary tract symptoms (LUTS) as the enlarging prostate begins to obstruct the urethra. Symptoms of BPH include:
Lower urinary tract symptoms (LUTS):
In advanced BPH, these LUTS may lead to complications such as:
Although benign prostatic hyperplasia is not cancerous, the LUTS symptoms may get severe and affect urination and daily life. If you are experiencing any of the urinary problems described above, it would be prudent to visit a doctor to discuss the possible causes of your symptoms as well as further treatment plans. Even if these symptoms are not bothersome, it is important to identify and rule out any underlying causes of LUTS.
Possible causes of LUTS may include:
If you experience acute urinary retention (sudden inability to pass urine and completely empty the bladder) seek medical attention immediately.
During your initial consultation, the urologist will discuss your symptoms and signs and will take a detailed medical history, including your family history and past medical history, so that they get a good understanding of your condition.
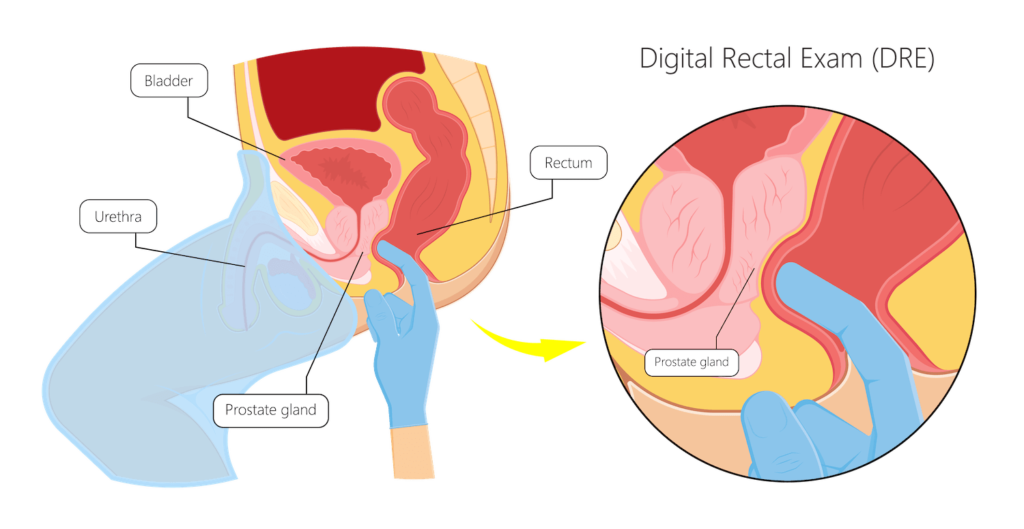
The urologist may also perform a physical examination to assess the cause of your symptoms. Physical examination usually includes abdominal and digital rectal examinations (see below). A brief neurological physical examination may also be performed if indicated.
Following this, further investigations may be required to confirm the diagnosis and rule out any complications. The majority of these diagnostic tests can be carried out in the clinic.
There are many ways to evaluate benign prostatic hyperplasia. These include:
The DRE is a fairly quick process where the doctor inserts a gloved, lubricated finger into the anus to examine the prostate gland’s posterior (back) wall.
The doctor will look out for any prostate enlargement, pain, and lumps/hard spots which may occur due to prostate cancer. A DRE usually lasts for about 20 seconds, and it is relatively painless, although some patients may experience slight discomfort. Overall, a DRE is an essential investigation in detecting any issues quickly and early.
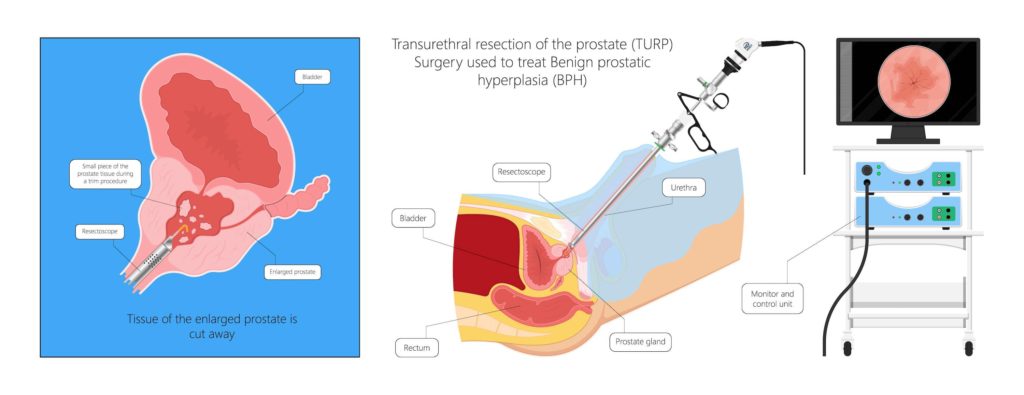
BPH leading to bothersome lower urinary tract symptoms can be treated in several ways, ranging from medical methods to surgery.
While many complications do not usually occur with benign prostatic hyperplasia treatment, some patients may face the following:
Painful urination or difficulty with urinating – While this may occur at the start of the treatment, symptoms will usually resolve with time. Some patients may even experience urinary retention, frequency, or urgency, but these effects are temporary and will return to normal after a few months.
Urinary tract infection (UTI) – Patients who struggle with urination or are not able to empty the bladder completely may have a higher risk of getting a UTI. Additionally, the use of catheters in a number of benign prostatic hyperplasia treatments may result in UTIs.
Bladder and kidney damage – If the patient is not able to empty the bladder properly, the wall of the bladder may weaken over time, and as a result, the bladder wall muscles may not be able to contract properly. This contraction is essential to pass urine. The pressure of an overly distended bladder due to not being able to urinate properly can damage the kidneys as well.
While there is no definite strategy to prevent BPH, adopting certain practices such as being more active, controlling type 2 diabetes, eating a well-balanced diet rich in fruits and vegetables, and limiting alcohol intake may have a positive impact on improving your urinary symptoms.
In conclusion, benign prostatic hyperplasia is a common condition among men as they age. Most men with an enlarged prostate do not develop many complications, and BPH can be readily treated with medication. If you suffer from BPH symptoms, ensure that you consult your urologist for a proper diagnosis and personalised treatment plan.

MBBS, MRCSed, MMED(Surgery)
Dr Terence Lim is a Senior Consultant Urologist with a subspecialty in Uro-Oncology. He is also the Medical Director at Assure Urology & Robotic Centre. His clinical interests include Uro-Oncology, Minimally-invasive Urological Surgery, Urinary Stone Disease, Endourology and Prostate Health.
Prior to his private practice, Dr Terence Lim spent almost two decades in public healthcare. He served as the Senior Consultant and Chief of the Department of Urology at Changi General Hospital (CGH). In addition, he is currently a Visiting Consultant at CGH. Dr Lim was also the director of CGH’s Advanced Surgical Centre, a committee dealing with complex surgeries, including robotic surgeries.
Your health is important to us and some conditions require immediate attention. For emergencies, please contact us at 9835 0668.

MBBS, MRCSed, MMED(Surgery)
Dr Terence Lim is a Senior Consultant Urologist with a subspecialty in Uro-Oncology. He is also the Medical Director at Assure Urology & Robotic Centre. His clinical interests include Uro-Oncology, Minimally-invasive Urological Surgery, Urinary Stone Disease, Endourology and Prostate Health.
Prior to his private practice, Dr Terence Lim spent almost two decades in public healthcare. He served as the Senior Consultant and Chief of the Department of Urology at Changi General Hospital (CGH). In addition, he is currently a Visiting Consultant at CGH. Dr Lim was also the director of CGH’s Advanced Surgical Centre, a committee dealing with complex surgeries, including robotic surgeries.
Your health is important to us and some conditions require immediate attention. For emergencies, please contact us at 9835 0668.
No issue is too small. Contact any of our friendly staff and we will get back to you as soon as possible.
Reach out to us for expert urological care.
For enquiries, leave a message and our friendly team will get in touch with you.
For urgent enquiries after office hours, call or WhatsApp us at (65) 9835 0668.
Monday – Friday: 9:00AM – 5:00PM
Saturday: 9:00AM – 12:30PM
Sunday & Public Holiday: CLOSED

© 2023 All Rights Reserved | Assure Urology & Robotic Centre | Terms & Conditions