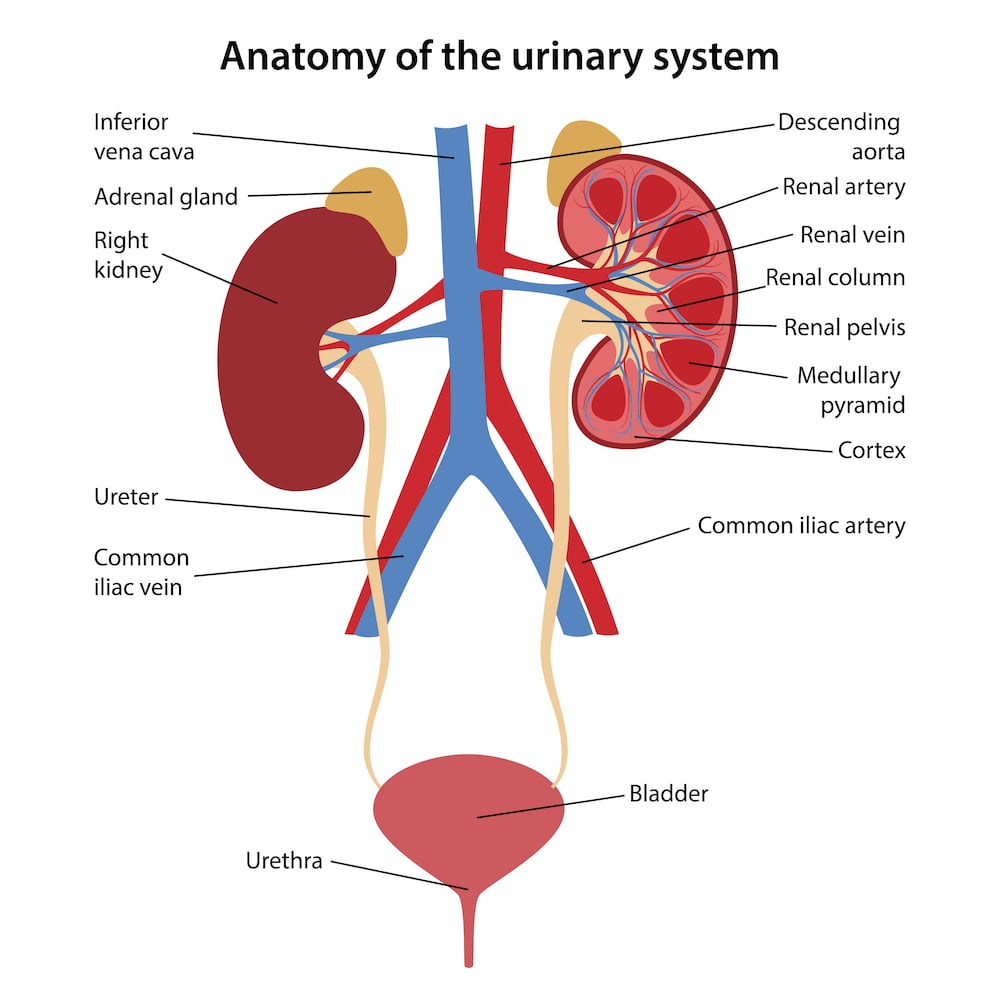
The bladder is a hollow organ found in our lower abdomen, and its main function is to store and expel urine. To do this, it has muscular walls that expand and contract to store and empty urine through the urethra.
Andropause (commonly termed ‘male menopause’) is a condition that involves a drop in testosterone levels in males and generally begins at the age of 40. This can cause a lowered sex drive, moodiness, and a variety of health issues, such as osteoporosis and metabolic syndrome.
Bladder augmentation is a type of surgery done for patients who do not have an adequate bladder capacity (i.e. bladder is unable to store as much urine as before), or in those whose bladder muscles do not stretch well due to disease conditions like previous radiation therapy. Bladder augmentation helps increase its size and capacity, and improves its ability to stretch.
Bladder augmentation is a complex reconstructive procedure that often involves using the body’s own tissue. This often comes from a section of the small intestine (ileocystoplasty) or the large intestine (sigmoid cystoplasty). Creating a larger bladder results in:
A patient who has a severe reduction in bladder compliance and/or bladder capacity may be a suitable candidate for bladder augmentation surgery. This surgery is usually only indicated in patients with severe symptoms or complications of bladder dysfunction and when all other less invasive treatments have failed. Conditions that may cause such bladder dysfunction include:
In children, conditions which cause neurogenic bladder are also why some children get bladder augmentation. Such conditions include:
These conditions will lead to sequelae such as urine leaks, bladder stiffness, loss of bladder capacity, and loss of bladder muscle function.
Before the surgery, the urologist will take a medical history from you as well as perform a physical examination and series of investigations. These investigations include blood tests to check your kidney function and overall health, as well as an array of other radiological investigations to look at your bladder and assess its function. Other tests include a urodynamic flow study to check for any abnormalities in urine flow (which can arise due to bladder dysfunction) as well as a cystoscopy, which involves the insertion of a long, thin, hollow tube at the end of it through the urethra and into the bladder, enabling the surgeon to visualise the inside of the bladder.
You will also have an appointment with the anaesthetist, a doctor in charge of administering anaesthesia to you during the surgery. The anaesthetist will take a further look at your medical history and background to assess your fitness and suitability for the operation. They may also advise you on what medications you can take and which you should stop (e.g. blood thinners like aspirin must be stopped a week before the surgery), as well as other lifestyle habits that will help minimise your risk of postoperative complications (e.g. to not smoke for at least 8 weeks before the surgery).
Bladder augmentation surgery s done under general anaesthesia, and the urologist can perform it either via the traditional, open surgery method (which involves a long cut down the centre of the abdomen) or through minimally invasive surgery, which involves either the use of robot-assisted surgery or laparoscopic surgery.
After the surgery, a catheter will be placed in your bladder to drain the bladder as it heals, as well as to allow for the washing of mucous and blood out of the bladder. Because a piece of the bowel is in contact with the bladder, you will need to irrigate the mucous regularly. You will be taught how to do this by nurses in the hospital before you are discharged. If irrigation is not done regularly, you may run the risk of bladder stones and a UTI.
Generally, bladder augmentation is only indicated when more conservative methods have failed. These could include medications such as oxybutynin, or minimally invasive methods such as the injection of medication or intermittent catheterisation.
You will not feel any pain during the surgery as you will under general anaesthesia. Post-operation, you may experience cramping in your lower belly and may be given medicine for one to two weeks.
Generally, the bladder can store up to 500ml for women and 700ml for men. However, we feel the need to urinate when the bladder is between 200-350ml full.
In some cases, the bladder needs to be completely removed (radical cystectomy). The creation of an ileal conduit involves surgically fashioning a tube from a piece of the small intestine (most often the ileum) to attach to the ureters & kidneys to allow urine to drain out of the body. The urine will then exit the body through a small opening in the skin, known as a stoma. After the surgery, the person will live with a urostomy bag that collects urine.
An ileal conduit is the most common form of urinary diversion performed by urologists after a patient undergoes a surgical procedure to remove the bladder. The ileum serves as an alternative pathway for the drainage of urine from the kidneys out of the body. Surgeries to remove the bladder are most often indicated in cases of cancer.
Some forms of these surgeries include:
The surgery can either be done via the traditional, open surgery method (which involves a long cut down the centre of the abdomen) or through a minimally invasive surgery which involves either the use of robotic surgery or laparoscopic surgery.
Similar to the aforementioned condition, a urology referral and check-up, as well as an appointment with the anaesthetist, will be conducted before the surgery.
The urologist will take a closer look at your medical history, and if you have cancer, they will also discuss at length with you the treatment options that are available. Because ileal conduits are often part of a major surgery, other surgeons, like a colorectal surgeon, may also be involved in the operation. You will be given advice on what medications to take and stop, what lifestyle measures to institute before the operation, as well as be given more information regarding the ileal conduit surgery.
Maintaining the ileal conduit will be a routine part of your everyday life. You will be briefed on how to look after your stoma properly. It is also important to help maintain your overall health after the surgery.
An ileal conduit acts as a diversion, making it possible for a person to drain urine out of their body after their bladder has been removed or damaged.
You will need to empty the bag every 2 or 3 hours, depending on how much you drink. A drainable ostomy bag allows you to empty the contents of your pouch and then reuse it.
Generally, urostomy bags should be replaced 1 to 2 times a week.
As the name suggests, neobladder reconstruction refers to the surgical construction of a “new bladder”. This is another option for urinary diversion, where the bladder is removed, and your urologist surgically recreates a new pouch to contain the urine. Usually, a piece of the small intestine is fashioned into the new bladder.
Patients with neobladder can generally urinate normally, often having to use abdominal muscles to empty the neobladder. Sometimes, a catheter may be used to empty the bladder.
Neobladder surgery is usually recommended for a person healthy enough for complex surgery. For example, one needs to have normal kidney and liver functions, and cannot have cancers in the urethra.
Contrary to popular belief, robotic surgery is not performed by a robot independently, but is performed by an experienced surgeon who guides the robot for the entire procedure via a console. These technological advancements allow for better visualisation, manual dexterity and control than what is possible with conventional techniques — a combination of the surgeon’s skill and critical thinking with the precision of a machine.
Furthermore, robotic surgery allows access to hard-to-reach areas using small incisions. This leads to a lower risk of complications and shorter recovery times.
Hopefully this has helped you better understand certain aspects of reconstructive bladder surgery and what it entails. Depending on your condition, your urologist will discuss the best method of urinary diversion for you.

MBBS, MRCSed, MMED(Surgery)
Dr Terence Lim is a Senior Consultant Urologist with a subspecialty in Uro-Oncology. He is also the Medical Director at Assure Urology & Robotic Centre. His clinical interests include Uro-Oncology, Minimally-invasive Urological Surgery, Urinary Stone Disease, Endourology and Prostate Health.
Prior to his private practice, Dr Terence Lim spent almost two decades in public healthcare. He served as the Senior Consultant and Chief of the Department of Urology at Changi General Hospital (CGH). In addition, he is currently a Visiting Consultant at CGH. Dr Lim was also the director of CGH’s Advanced Surgical Centre, a committee dealing with complex surgeries, including robotic surgeries.
Your health is important to us and some conditions require immediate attention. For emergencies, please contact us at 9835 0668.

MBBS, MRCSed, MMED(Surgery)
Dr Terence Lim is a Senior Consultant Urologist with a subspecialty in Uro-Oncology. He is also the Medical Director at Assure Urology & Robotic Centre. His clinical interests include Uro-Oncology, Minimally-invasive Urological Surgery, Urinary Stone Disease, Endourology and Prostate Health.
Prior to his private practice, Dr Terence Lim spent almost two decades in public healthcare. He served as the Senior Consultant and Chief of the Department of Urology at Changi General Hospital (CGH). In addition, he is currently a Visiting Consultant at CGH. Dr Lim was also the director of CGH’s Advanced Surgical Centre, a committee dealing with complex surgeries, including robotic surgeries.
Your health is important to us and some conditions require immediate attention. For emergencies, please contact us at 9835 0668.
No issue is too small. Contact any of our friendly staff and we will get back to you as soon as possible.
Reach out to us for expert urological care.
For enquiries, leave a message and our friendly team will get in touch with you.
For urgent enquiries after office hours, call or WhatsApp us at (65) 9835 0668.
Monday – Friday: 9:00AM – 5:00PM
Saturday: 9:00AM – 12:30PM
Sunday & Public Holiday: CLOSED

© 2023 All Rights Reserved | Assure Urology & Robotic Centre | Terms & Conditions